Explore the relationship linking Alcohol Use Disorder and sleep apnea in veterans, their developmental contributing factors, and some management or treatment strategies.
The reintegration process of veterans into civilian life is accompanied by various health challenges. AUD and sleep apnea are two important, often overlapping issues. These conditions have serious effects on the quality of life, health, and well-being in general. The two most common conditions among veterans that have a very negative impact on quality of life include alcohol use disorders and sleep apnea. Both are, logically, concurrently present, thereby worsening the situation due to their ability to get engaged in a self-reinforcing cycle of symptoms exacerbation and therefore complicate therapy.
Understanding Alcohol Use Disorder and Sleep Apnea
Alcohol Use Disorder (AUD)
AUD is a chronic, relapsing brain disease characterized by compulsive alcohol seeking and use despite the involved harmful consequences. AUD has been more prevalent in veterans in comparison to other populations due to the stressful exposure that some may have undergone during their service.
Sleep Apnea
https://trendydiet.me/indian-spices-names-in-english-and-hindi/Sleep apnea is a kind of sleep disorder characterized by breathing pauses while one is asleep. It can cause excessive sleepiness during the day, fatigue, and many other health complications. Veterans are at an increased risk of sleep apnea resulting from factors such as obesity, smoking, and hazardous substance exposure.
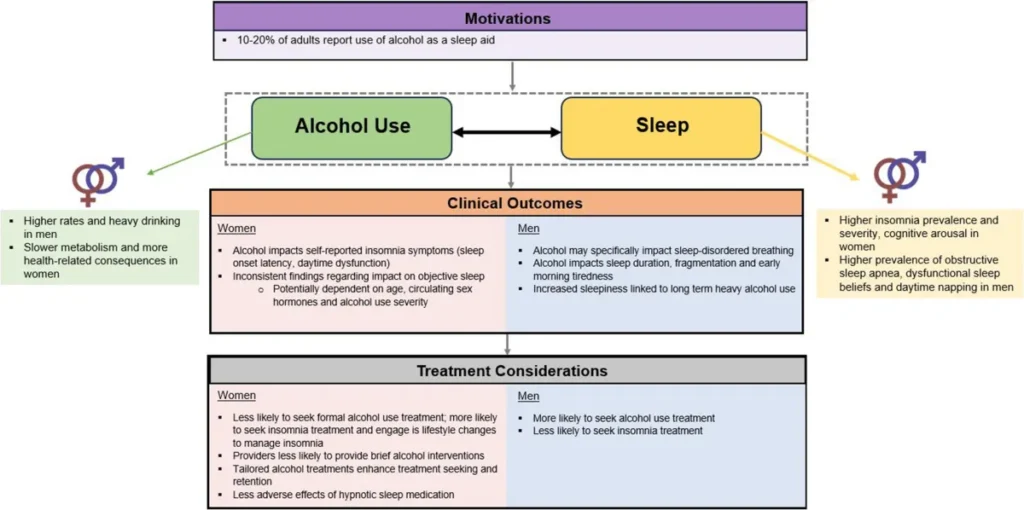
Relationship Between AUD and Sleep Apnea
The relationship between AUD and sleep apnea is complex and bidirectional.
AUD Can Contribute to Sleep Apnea: Alcohol consumption is known to interfere with sleep patterns, and this can cause sleep apnea. It may relax the throat muscles as well, which in turn increases the risk of the airway collapsing.
Sleep Apnea Can Aggravate AUD: Conversely, sleep apnea will contribute to bad sleep quality, leading to irritability, mood swings, and increasing cravings for alcohol. This causes hardship for veterans who are working to control their AUD.
Factors of AUD and Sleep Apnea in Veterans
Causes and Risk Factors of AUD
The following are some of the factors that might increase the risk of AUD for veterans:
Combat Exposure: It may lead to PTSD and other mental health issues, raising the risk of falling to alcohol as a self-prescribed cure.
Chronic Pain: Service-related injuries or conditions lead to chronic pain for most veterans, leading to possible self-medication with alcohol
Social Isolation: Difficulty adjusting to civilian life places one in social isolation, increasing their consumption of alcohol
Symptoms and Diagnosis
The symptoms of AUD vary but overall include:
Increased Tolerance: Characterized by the need for a person to drink more to feel the same effects.
Withdrawal Symptoms: Development of such symptoms as tremors, anxiety, or nausea when not drinking.
Neglecting Responsibilities: Continuing to use alcohol despite failure to fulfill major role obligations at work, school, or home.
In most cases, diagnosis requires an individual to see a health professional who will conduct a full assessment, including self-reported questionnaires and interviews.
Treatment and Management
The following are common ways of treating AUD in veterans:
Therapy: Treatment, such as cognitive behavioral therapy and other forms of behavioral treatment, can uncover the AUD’s underlying issues and learn healthier ways of dealing with them.
Medication: Medications such as disulfiram, naltrexone, and acamprosate reduce cravings and relieve withdrawal symptoms.
Support Groups: Support groups like AA keep the individual responsible for actions and provide a platform for peers who understand the daily struggles involved with this addiction.
Holistic Care: Treating co-occurring disorders, such as PTSD or chronic pain, is integral to overcoming AUD.
Screening for Sleep Apnea in Veterans
Sleep apnea is a disorder characterized by recurring interruption of breathing at one time during sleep. It majorly causes poor sleeping quality and related daytime fatigue, among many other health complications. Veterans are exposed to an increased risk of developing sleep apnea, which can be further enhanced by their lifestyle and their physical health conditions.
Causes and Risk Factors of Sleep Disorder
Several factors contribute to a higher prevalence of sleep apnea among veterans:
Obesity: It is one of the most prominent reasons behind sleep apnea. Thus, veterans may be inflicted with it as well. PTSD: This contributes to sleep pattern disturbance and leads to susceptibility to sleep apnea. Chronic Health Conditions: Circulatory disorders, hypertension, and cardiovascular diseases, which are pretty common in veterans, are the related conditions to sleep apnea as well. Symptoms and Diagnosis The most common signs and symptoms of sleep apnea are mentioned below :
Loud Snoring: Loud, frequent snoring is often symptomatic of OSA.
Gasping for Air: Waking up suddenly with a choking or gasping sensation.
Daytime Sleepiness: Excessive daytime fatigue or sleepiness despite sleeping at night.
Confirmation of the diagnosis requires a sleep study, usually done in a sleep clinic or, more recently, with portable equipment at home.
Treatment and Management of Sleeping Disorder
The various treatment modalities for sleep apnea are:
Continuous Positive Airway Pressure: It is the most common and productive treatment. It involves the operation of a machine that helps keep one’s airway open during sleep.
Changes in Lifestyle Habits: Weight loss, aversion to alcohol, and sleeping on one’s side may help.
Surgery: This could be considered in extreme cases where there is a need for surgically removing or lessening the excess tissue that blocks the airway passage.
Bidirectional Relationship Between Alcohol Use Disorder and Sleep Apnea
There is a bidirectional relationship between alcohol use disorder and sleep apnea. Alcohol use can worsen sleep apnea, and conversely, untreated sleep apnea can predispose to alcohol misuse.

How Alcohol Affects Sleep Apnea
Relaxation of Airway Muscles: The alcohol relaxes the throat muscles involved in breathing, which is a factor that may promote airway obstruction during sleep.
Disrupted Sleep Architecture: Alcohol interferes with the normal sleep cycle, reducing its quality and exasperating the effects of sleep apnea.
Apnea Events of Higher Severity: The intake of alcohol can raise the frequency of apneic events and their severity, both events contributing to a decrease in the quality of sleep and increased somnolence during the day.
How Sleep Apnea Contributes to Alcohol Misuse
Fatigue and Mood Disturbances: Fatigue and irritation from sleep apnea could contribute to veterans using alcohol as a way to cope.
Disrupted Sleep Patterns: Poor quality sleep due to apnea could exacerbate alcohol craving and use, where individuals self-medicate to improve their sleep disturbances.
Increased Stress: Increased chronic stress from sleep deprivation can add to higher alcohol consumption rates.
Consequences of Co-occurring AUD and Sleep Apnea on Veterans
The co-occurrence of AUD and sleep apnea will significantly impact veterans’ lives about the following issues:
Quality of Life: Quality of life is reduced for those who have AUD and sleep apnea. It can lead to fatigue, excessive daytime sleepiness, and problems with concentration and attention.
Increased Risk of Mishaps: Excessive daytime sleepiness increases the chances of falling asleep while driving or operating heavy machinery at work, which in turn may cause mishaps.
Mental Health Problems: AUD and sleep apnea can cause depression, anxiety, and other mental health problems.
Physical Health Problems: Both can contribute to raised risks for cardiovascular diseases, stroke, and other medical issues.
Traumatic Brain Injury (TBI): The risk of AUD and sleep apnea is highly enhanced in Veterans with TBI.
Post-Traumatic Stress Disorder (PTSD): In an effort to self-medicate, a Vet with PTSD might turn to alcohol, which would further disrupt sleep patterns.
Exposure to Hazardous Substances: During military service, one may be exposed to hazardous materials that increase the potential risks for AUD and sleep apnea.
Genetics: A family history of AUD or sleep apnea can increase a person’s risk of developing these conditions
Treatment of Alcohol Use Disorder and Sleep Apnea in Veterans
AUD and sleep apnea require an integrated approach to treatment and management that addresses both problems at the same time in order to be effectively treated and managed in veterans.
Cognitive-Behavioral Therapy: A system where the coping skills of veterans are improved in evaluating and resituating the craving and triggers of AUD.
Medication-Assisted Treatment: It could be an effective treatment for AUD, and it is especially effective with some forms of counseling and therapy.
Continuous Positive Airway Pressure: It is the gold standard of treatment for sleep apnea, involving a pressurized mask that gives airflow through a mask, which one sleeps in to hold the airway open.
Lifestyle Modifications: Some common ways to manage AUD and sleep apnea are changes in alcohol avoidance, regular exercise, and a healthy diet.
Support Groups: It provides a platform where veterans can share their feelings with others, thereby gaining emotional support and encouragement.
Treating Both Conditions Concurrently
Treatment of both AUD and sleep apnea must therefore be integrated to treat both issues at the same time.
Biopsychosocial Intervention Methods
Full Assessment: Identifying and addressing both AUD and sleep apnea through a full assessment by health professionals is very essential.
Coordinated Care: Addiction specialists, doctors in sleep medicine, and primary care providers can coordinate in providing an integrated approach to treatment.
Behavioral Interventions: Such behavioral interventions may help deal with alcohol abuse and sleep-related disorders, as indicated by cognitive-behavioral strategies for conducting interventions related to managing cravings and sleep hygiene.
Management of Both Disorders
Abstinence from Alcohol: Decreased consumption or total abstinence from alcohol markedly improves the symptoms of sleep apnea.
Good Sleep Hygiene: Maintenance of sleep schedules, sleep-conducive environment, and avoidance of stimulants before going to bed are some strategies to conduct good sleep hygiene.
Monitor and adjust treatment: Follow up with health providers for the needful adjustment in the treatments related to AUD and sleep apnea.
Resources and Support for Veterans
Veterans facing alcohol use disorder and sleep apnea can avail of the following resources and support systems that would help in their recovery process:
Veterans Affairs Programs: The VA has specially developed programs and services for veterans suffering from AUD and sleep apnea. These will include counseling and treatment programs and sleep studies.
Support Groups: Groups like AA, and support groups on sleep disorders, provide peers and real-life experience-based advice.
Websites and online forums are other internet resources that can help one when dealing with AUD and sleep apnea.
Conclusion
Alcohol use disorder and sleep apnea are two major health concerns for veterans, often overlapping to complicate one another. An interrelationship between these disorders, sometimes extremely complex, holds the key to their effective management and treatment. Better health and quality of life may be attained by focusing on an integrated approach: comprehensive assessment, behavioral interventions, and coordinated care for the two disorders for veterans.
First of all, if you or the veteran in your life battles alcohol use disorder, sleep apnea, or both, look for professional help; it is the first step to recovery. Making use of resources and support systems available for these conditions will enable one to better manage such conditions and, finally, attain a healthier and more complete life.
